Dear SDCOS Friends, Happy 2026! I hope that everybody had an enjoyable holiday season and is transitioning smoothly into the new year. For this month’s Retina Corner, I will be sharing an interesting retinal vein occlusion case from my clinic.
Case Presentation:
An 67-year-old female presented with painless decreased vision in her left eye that she had noted over 2 weeks prior. She had a history of systemic hypertension and pre-diabetes mellitus. 20/20 in the right eye and 20/30 in the left eye. Her IOP was normal in each eye. There was no relative afferent pupillary defect and confrontational visual fields were intact in both eyes.
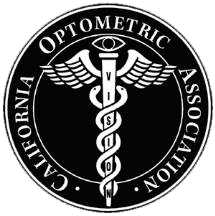
Her funduscopic exam demonstrated a normal appearing right eye and scattered retinal hemorrhages in the left eye with mild venous engorgement and no cotton-wool spots or disc edema (Figure 1A, B). The retinal hemorrhages showed up as scattered foci of hypoautofluorescence on fundus autofluorescence imaging (Figure 1C).
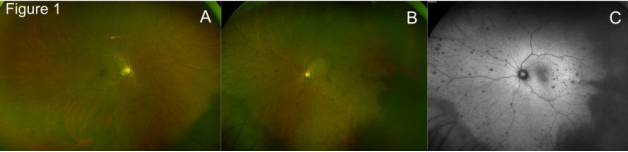
There was no evidence of cystoid macular edema or retinal thickening on OCT imaging in either eye (Figure 2A, B).
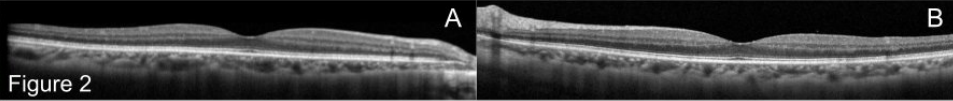
Fluorescein angiography of the left eye demonstrated normal transit of dye, blockage of signal from the scattered retinal hemorrhages but no evidence of non-perfusion, scattered peripheral microaneurysms and mild late disc leakage (Figure 3).
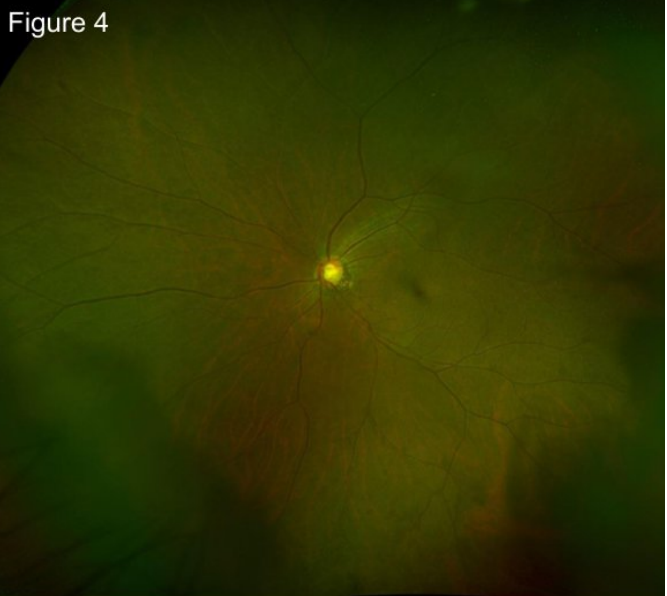
The patient was diagnosed with a non-ischemic central retinal vein occlusion and advised to follow-up with her primary care doctor for hypercoagulability studies, which were negative as well as blood pressure, cholesterol and blood glucose monitoring. 3 months after her initial presentation, she returned with subtle improvement in vision (20/25 ph 20/20) and complete resolution of her retinal hemorrhages (Figure 4).
Discussion:
Central retinal vein occlusion (CRVO) is the second most common cause of vision loss due to retinal vascular disease, following diabetic retinopathy. The underlying causes of CRVO typically involve a combination of systemic and local factors leading to venous obstruction. Most commonly, CRVO results from thrombosis within the central retinal vein, often precipitated by conditions such as hypertension, diabetes, and hyperlipidemia. These systemic diseases can lead to endothelial dysfunction and increased vascular permeability, promoting a pro-thrombotic state. Additionally, anatomical variations, such as the presence of a narrow angle between the artery and vein at the optic disc, can contribute to mechanical compression of the vein, further increasing the risk of occlusion.
CRVO can be classified into two main categories: ischemic and non-ischemic. Ischemic CRVO is characterized by a more severe form of retinal damage and is often associated with a greater risk of complications, such as neovascularization and significant, permanent vision loss. In contrast, non-ischemic CRVO, as observed in our case, typically presents with milder symptoms and a better overall prognosis. The distinction between these two types is primarily based on the presence of retinal ischemia, which can be assessed through multimodal imaging techniques such as OCT, OCTa, and fluorescein angiography or suggested by clinical features such as cotton wool spots and disc edema.
In the management of CRVO, treatment options vary depending on the type and severity of the occlusion. For non-ischemic CRVO without CME, observation following complete work-up is often sufficient, as many patients experience spontaneous resolution of retinal hemorrhages and gradual improvement in vision, as demonstrated in the case presented. In contrast, ischemic CRVO may necessitate more aggressive interventions, including intravitreal injections of anti-VEGF agents, corticosteroids, or laser photocoagulation to treat and prevent complications.
A comprehensive work-up for CRVO should include a thorough history and examination, along with close follow-up with a primary care provider and pertinent lab tests to identify underlying systemic conditions such as hypertension, diabetes, or hypercoagulable states. The prognosis for non-ischemic CRVO is generally favorable, with many patients achieving significant visual recovery over time, as seen in the 3-month follow-up of our patient.
I hope that you enjoyed this month’s edition of Retina Corner. As always, if you have any questions or there is ever something I can help with, please feel free to contact me at any time. I am also open to any requests, if there is a topic or case that you would like for me to discuss in this space.
Best wishes, and until next time,
Thomas Lazzarini, MD
Retina Consultants San Diego
626-537-5857 (cell)
lazzarini@rcsd.com